Frontline medics: Immunoglobulin can prevent COVID-19 patients turning critical
- By Zhu Bochen
 0 Comment(s)
0 Comment(s) Print
Print E-mail China.org.cn, May 12, 2020
E-mail China.org.cn, May 12, 2020
A team from the Peking Union Medical College Hospital (PUMCH) have suggested using immunoglobulin and low-molecular-weight heparin (LMWH) to prevent COVID-19 patients from turning critical.
Professor Li Taisheng, director of the Infectious Disease Department at PUMCH, and his team applied this treatment to nearly 30 patients in Wuhan, and found that it could effectively stop patients from developing critical complications such as multiple organ dysfunction or failure and respiratory failure.
"During a severe viral infection, a high dose of immunoglobulin can shut down the inflammatory cascade, and help improve humoral immunity," Li explained during an online lecture in April.
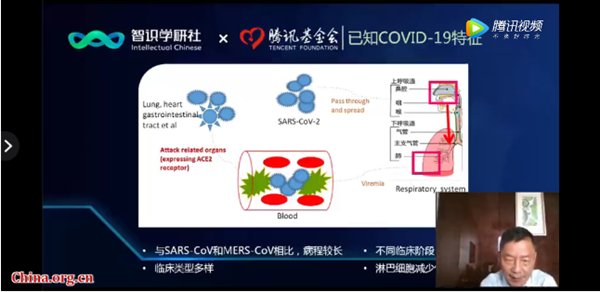
Through clinical observation and research, Li and his team discovered various differences between COVID-19 and Severe Acute Respiratory Syndrome (SARS).
According to Li, COVID-19 patients usually suffer from damage to multiple organs and body systems while developing a diverse set of symptoms that can be hard to detect. It also takes a comparatively longer time for COVID-19 patients' immune cells to recover.
Based on this conclusion, Li and his team conducted a randomized clinical trial using a high dose of immunoglobulin among critically ill COVID-19 patients in Wuhan. The result turned out to be effective, especially to those who developed symptoms within two weeks.
In addition to the treatment methods, Li's team also listed several significant laboratory markers indicating when COVID-19 patients turn from mild to critical.
"These include a significantly elevated level of C-reactive protein, ferritin, as well as interleukin-6 in some cases. Meanwhile the increase of these inflammatory proteins often comes with a continuous decrease of lymphocyte." Li elaborated.
As for the triggers of this turning, Li said that patients with advanced age and other medical records such as diabetes, hypertension, and tumors were at the highest risk.
Li and his team further put forward a hypothesis on COVID-19 complications, in which patients often experience three major stages.
"The first stage is called viremia, and it usually lasts for seven days while patients only develop mild symptoms. If without any of these aforementioned triggers, patients could recover via their own immune system." Li explained. "Otherwise, patients are likely to enter the so-called acute phase after one week."
During the acute phase, patients will experience a decrease of B-cells and T-cells (lymphocytes). "We can only provide passive treatment for them, such as providing oxygen supplies and ventilators, so the fatality rate is rather high at this stage." Li noted.
"According to our hypothesis, we should then apply a high dose of immunoglobulin and LMWH to patients at high risk of turning critical within two weeks of them starting to show COVID-19 symptoms."
During a Q&A session, Li shed light on the lessons he had learnt as one of the frontline medics in Wuhan. "Since the specific cure for COVID-19 hasn't yet been developed, I believe we should attach great importance to precautionary methods at the earliest stage." Li suggested.
"That being said, we should work to detect infected cases and conduct isolated observation as early as possible." Li said. "Doctors should be fully aware of the possible triggers that might put patients into critical condition, and conduct treatment accordingly."
For those who turn critical, Li added that the plasma therapy might be the most effective treatment currently. "Ventilators are also important for them, but we must avoid infection in this regard, and conduct anti-biotics treatment for them as early as we can."





